- Country Areas
- Methods and indices
- Explore oral health
- About CAPP
-
- Bank of Ideas
- Nepal - Basic Oral Health Training Programme for the Health Workers of Ramechhap District
- Nepal - Manang Dental Camp Report
- Nepal - School based oral health project in remote Timal Besi
- Nepal - Training Female Community Health Volunteers in Oral Health Education
- United Kingdom - Fissure Sealant Programme for Schoolchildren in Wales
- United Kingdom - Boost Better Breaks - A School based Public Health Programme in Northern Ireland
- United Kingdom - Training programme for nursing staff on oral health care of elderly residents of nursing homes in Scotland
- United Kingdom - An Oral Cancer Awareness Campaign Programme, Scotland
- United Kingdom - Designed to Smile - Promoting Better Oral Health and Delivering Fluoride Supplementation to Children in Wales
- United Kingdom - Childsmile – the national child oral health improvement programme for Scotland
- Sweden - A school-based fluoride mouth rinsing programme
- Kenya - The Eric Dental Clinic
- Madagascar - The Vezo Hospital
- Nigeria - A School based oral health education programme for Children
- Seychelles - Dental Public Health Programmes
- South Africa - Hammanskraal Project
- South Africa - Phelophepa Healthcare Train
- Afghanistan - Dental Relief Project, Kabul
- Australia - Water fluoridation in remote Aboriginal communities
- Australia - An Aboriginal health and a Government school dental service in South Australia
- Austria - Oral Health Promotion Programme for preschool children, Vorarlberg
- Antigua and Barbuda - School based Fluoride rinse programme, 1989-1998
- Brunei Darussalam - Mission Report 1998 on training course in oral health survey method
- Cambodia - Mobile dental care for schoolchildren in Sihanoukville
- Cambodia - Outreach programme for improving oral health of under privileged children in Sihanoukville
- Cambodia - Oral Health promotion in schools in Kampong Cham
- Namibia - The "Smiling Schools" project
- South Africa - An Atraumatic Restorative Treatment (ART) Project: Activity Report
- South Africa - An Atraumatic Restorative Treatment (ART) in a Mobile Dental Clinic, Johannesburg
- Tanzania, United Republic of - The Outreach programme in primary schools around the Dar es Salaam area
- Argentina - An Oral Health Preventive Programme for School Children
- Brazil - Atraumatic Restorative Treatment for a disadvantaged Brazilian Community
- Chile - A school based oral health programme in Cabildo (2008)
- Chile - Fluoridated milk programme for rural primary school children
- Chile - Fluoridated Powdered Milk Programme
- El Salvador - Community-based programme for prevention of dental caries among children
- Honduras - Oral Health Education and Care for a resource poor Honduran community
- Honduras - Oral Health and Care in Delicias
- United States of America - Oral Health Programme for Navajo Indians in Pine Hill, New Mexico
- United States of America - Oral health Education and Sealant programme for West Philadelphian Schoolchildren
- Kuwait - A school based oral health programme during 1986-1997
- Kuwait - Community Based Schoolchildren's Oral Health Programmes 1985 -1998
- Kuwait - School Oral Health Programme (1982-2011)
- Lebanon - Final Report, a baseline survey of oral health situation and fluoride levels in drinking water (2000)
- Saudi Arabia - An ongoing oral health promotion programme
- Saudi Arabia - The Celebration of the 20th anniversary of the accession to the throne of King Fahd Ibn Abdul-Aziz
- Saudi Arabia - Oral Health Education Programme for schoolchildren in the Holy City of Mecca
- Sudan - An Oral Health Promotion through live art in Sudan
- Syrian Arab Republic - An ongoing oral health preventive programme
- United Arab Emirates - Assignment Report 1995-96 with recommendations to build a comprehensive oral health care
- United Arab Emirates - Dental Public Health Programs implemented by Dental Services Department, Dubai
- United Arab Emirates - MY SMILE” - tooth brushing program for school children in Dubai, UAE.
- Bulgaria - A community based milk fluoridation programme 1988-1993
- Bulgaria - The clinical effect of milk fluoridation for school children
- Croatia - Healthy Smile Day
- France - A School Based Oral Health Education Programme
- Germany - Third German Oral Health Study - 1997, Summary
- Germany - An Oral health programme for children attending kindergartens in two Counties in Northern Hesse
- Romania - Fluoride mouth rinsing Programme in Schools in Constanta and Iasi connties (2001-2010)
- Russian Federation - Programme focusing educating parents of infants on the prevention of caries, Moscow
- Sweden - An oral health programme for preschool children in a multicultural city area
- Sweden - The Oral Health Lift - An Oral Health Promotion Programme for the Homeless and other socially vulnerable people in Malmö
- Sweden - School based fluoride varnish application programme
- Turkey - Ongoing Atraumatic Restorative Treatment (ART) Programme in some rural areas
- Turkey - A reliable and practical dental preventive/education program model for Turkey - "brushes in the bags, teeth on the healthy-way"
- India - Training oral health workers to provide basic dental care in Ladakh
- Indonesia - Affordable toothpaste project (WHO) in West Kalimantan
- Sri Lanka - School based public health programme in Jaffna
- Sri Lanka - ART Training Programme for School Dental Therapists, Jaffna
- Sri Lanka - An oral cancer screening project in tea estates
- Sri Lanka - Oral Health Camp in rural area
- Sri Lanka - Dental public Health Programmes conducted by the Population Oral Health Unit (Community Dental Unit), Dental Institute, Colombo
- Thailand - The Royal Mobile Dental Unit project
- Thailand - School based oral health programme for children in Southern Thailand
- China - A campaign on "Love Teeth Day" celebrated nation-wide each year
- China - Milk fluoridation project (WHO) in Beijing
- China - An oral health education programme in Wuhan City
- China - An oral health education and supervised tooth brushing programme in kindergartens
- Japan - A school-based fluoride mouth rinse programme for preschool children
- Japan - Visual Support Material for Children with Autism in order to Master Toothbrushing Skills
- Viet Nam - School-based Oral Health Programme
- Viet Nam - Mission report 1999 with recommendation for oral health training
- Viet Nam - Oral health program in South Central Vietnam
- Vanatu - Mission Report on Oral Health
- Tonga - Mission Report 1997 reviewing the oral health programme
- Tokelau - Mission Report 1999 on recommendation to improve oral health
- Philippines - Mission Report 1998 on planning and implementing a national oral health survey
- Philippines - The Essential Health Care Package- “Fit for School” programme
- Mongolia - Mission Report 1999 with recommendations to improve oral health (1)
- Malaysia - reports from Oral Health Division
- Lao PDR - Caries prevalence and some caries related factors for 12-year-old children from Vientiane and Luang Prabang provinces
- Lao PDR - Estimating the fluoride concentration in the drinking waters
- Korea, Republic of - Community based caries prevention programme in a suburban area
- Sri Lanka - An ongoing school-based ART Programme
- Vanuatu - Gudfala Tut Skul Program (Healthy Tooth School Program)
- Estonia - Suukool, a mouth school
- Palestine - Integrating the WHO Health Promoting School Concept into National School Oral Health
Palestine - Integrating the WHO Health Promoting School Concept into National School Oral Health
Palestine - Integrating the WHO Health Promoting School Concept into National School Oral Health
Dr Lamis Abuhaloob WHO CC for Public Health Education and Training, Imperial College London, London, United Kingdom
Professor Poul Erik Petersen WHO Collaborating Centre for Community Oral Health Programmes and Research, University of Copenhagen, Denmark
Introduction
The Palestinian Territories comprise two geographically separated areas (Figure 1): West Bank (WB) and Gaza Strip (GS). The WB comprise an area of 5,800 km2 west of the River Jordan. The GS is a narrow strip of highly populated land of 360 km2 lying on the eastern coast of the Mediterranean Sea1. The WB and GS contain 16 and 7 governorates, respectively2.
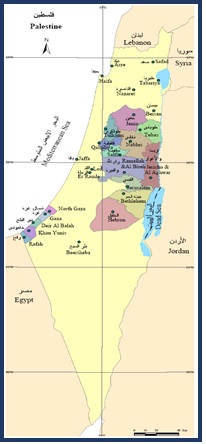
Figure 1. Map of Palestinian Territories
The long-term political instability in the Palestinian territories has caused serious deterioration of socioeconomic conditions. In addition, because of financial limitations existing health services are unable to meet the population’s oral healthcare3. This is the first national oral health promotion study in Palestine applying the principles of the WHO Health Promoting Schools concept4 at the national level and involved representative governmental primary schools from all governorates.
Background and rationale
During the past 15 years, the burden of dental caries has been persistently high among 6-year-old children and a considerable increase in caries prevalence is now prominent among adolescents5, 6. In 2017, 83.4% of Palestinian grade 1 children suffered from dental caries in primary teeth and the average dental caries experience was dmfs 11.27.
'Research carried out in the Palestinian territories has identified substantial social risk factors important to children’s health including constrained economic resources of families, poor health-related quality of life, residing in refugee camps, poor nutrition status, the experience of governmental instability, and severe barriers to accessing healthcare services.
Although most recent research reported high dental care awareness among Palestinian mothers, the risk of dental caries remains high in Palestine because of irregular dental visiting practices, infrequent tooth brushing habits, low exposure to fluoridated toothpaste, and elevated sugar consumption7.
The School Health Programme was established in 1994 by the Ministry of Health and United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA) in order to provide dental care for children enrolled in governmental private schools in the Gaza Strip and the West Bank and refugee’s settings (UNRWA). This programme should include oral health screening, referral for dental care, follow-up services, oral health education and oral health promotion8. However, the existing school dental health programme does not match the oral health needs and an organized oral disease prevention programme would be important for tackling the poor oral health situation of Palestinian children.
Aims and objectives
This project aimed to develop and implement a demonstration programme for the promotion of oral health among primary schoolchildren in a representative sample of primary schools in Palestine. The project applied the principles of the WHO Health Promoting Schools concept4 which involves the creation of classroom-based health education to be carried out by schoolteachers coupled with family and community actions9.
Project Outline
A quasi-experimental study (2016-2018) recruited 3939 schoolchildren aged 5-6 years from 30 intervention schools (n=2333) and 31 comparison schools (n=1606). At baseline and post-intervention, mothers and schoolteachers completed WHO self-administered questionnaires about the oral health of children, oral health behaviour, and family factors. A total of 25 calibrated dentists examined the dental caries of children according to WHO criteria. Trained teachers in the intervention schools provided comprehensive oral health education to children in the classrooms, held regular oral health sessions for mothers, and supervised children's daily toothbrushing with fluoride-containing toothpaste (1,450 ppm F) at school.
The project implementation process is summarised in Figures 2, 3, 4, 5 and 6.
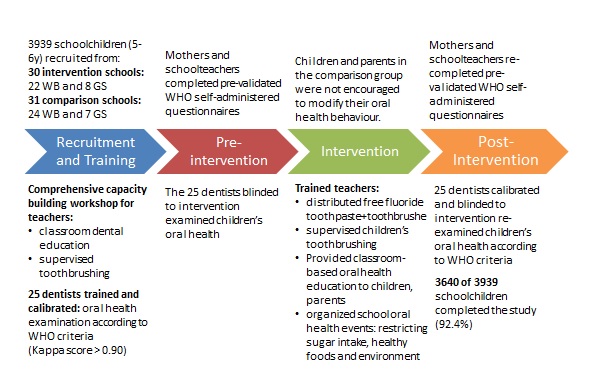
Figure 2. Chart describing Palestinian school oral health project implementation process
Figure 3: Teachers’ capacity building and dentists' training workshops in the Ministry of Health and Ministry of Education in Palestine
Figure 4. School oral health dentists examine Palestinian children’s oral health based on the WHO criteria


Figure 5. Trained teachers provide classroom-based oral health education to children and parents in Palestine


Figure 6. Trained teachers distribute fluoride toothpaste and toothbrushes free of charge and supervise children’s daily toothbrushing
Achievements
After 24 months of the programme implementation, the follow-up was completed for 75.8% of recruited children. The results showed that dental caries experience declined over the project, in both dentitions. The reduction in DMFT and DMFS was 23.3% and 23.2% (P<0.001), respectively. The drop-in caries experience indices in Gaza Strip were four to eight times higher than in West Bank and reached a 47.4% reduction in DMFT (Figure 7)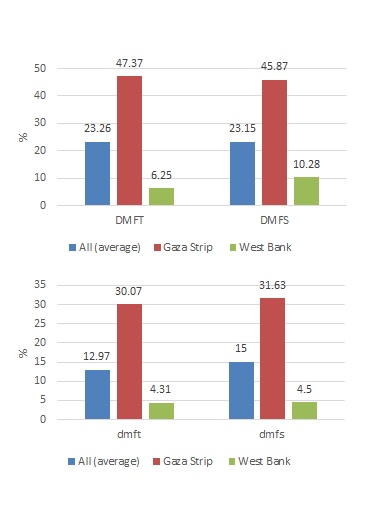
Figure 7. Reduction (%) in dental caries experience of schoolchildren in intervention collaborative schools compared to control schools (P<0.001)
In the intervention group, fewer children avoided smiling, fewer children missed classes because of toothache and 40% of children visited a dentist once or twice a year. The main reason for visiting the dentist was pain/troubles with teeth or gums. The percentage of children practicing toothbrushing at home two or more times a day increased, and 72.5% of the children used fluoride-containing toothpaste.
For 76.9% of 6-years old schoolchildren in the intervention schools, parents were the main source of information on oral healthcare. The contribution of teachers to oral healthcare facts raised to 43.3% in the intervention group by the end of the study (Figure 8).
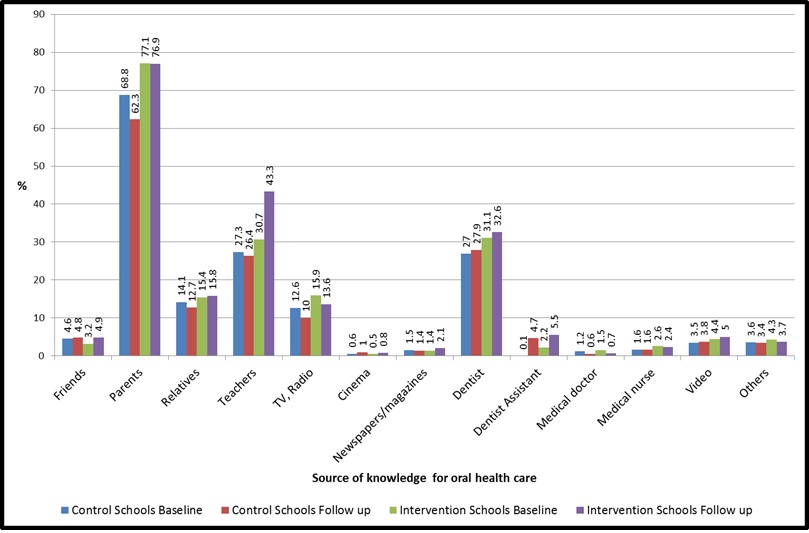
Figure 8. Source of knowledge for oral health care for 5-7-years old schoolchildren, at baseline and after 24 months
Mothers and teachers showed improvement in knowledge and positive attitudes towards dental care. The involvement of schoolteachers in oral health in schools and acceptance of dental health education materials significantly enhanced children’s oral health behaviour.
The WHO school oral health promotion programmes implemented in primary schools in Thailand10 and China11 showed a similar outcome.
Constraints
Palestine has suffered from long-lasting political unrest for decades. The implementation difficulties observed in this study mostly relate to bureaucratic governmental procedures and political unrest. The field control of the project was better in the GS due to enhanced access to schools since there were no Israeli checkpoints. These checkpoints in the WB area were hugely delaying programme undertakings. Meanwhile, the Ministry of Health in Palestine was unable to support the entrance of the project Principal Investigator in regular travels from the GS to WB areas. Such obstacles emphasize the necessity of effective collaboration with WHO and UNICEF to facilitate the movements of researchers in occupied regions and to ensure the implementation of national health promotion projects appropriately.
Conclusion
The school-health intervention was effective in preventing up to 47.4% of dental caries incidents. However, the effectiveness varied between different geographic parts of Palestine because of differences in tap water fluoride concentration level (GS 1.38 and WB 0.24), field control, system administration procedures, and political unrest. Community support by international health associations may facilitate oral health programme implementation in politically distressed regions. In addition, this study confirmed the experience of empowered parents, schoolteachers and the community at large in disease prevention in poor settings. Finally, effective results in dental caries prevention are particularly obtainable when disease prevention programmes involve toothbrushes free of charge and fluoridated toothpaste.
Acknowledgements
Sincere thanks to the Borrow Foundation for having provided valuable funds for the project. Genuine thanks to the Ministry of Health and Ministry of Education in the State of Palestine for their significant help and contribution in implementing and running the projects.
References
- Shomar BH, Müller G, Yahya A. Seasonal Variations of Chemical Composition of Water and Bottom Sediments in the Wetland of Wadi Gaza, Gaza Strip. Wetlands Ecology and Management 2005; 13(4):419-31, Ministry of Health. The Status of Health in Palestine: Annual Report 2005. Palestine: Ministry of Health-Health Management Information System, 2006
- Ministry of Education. Education Statistical Yearbook 2012/2013. Pamallah, Palestine, 2013
- Ministry of Health. The Annual report of Oral Health Department. Palestine: Ministry of Health-Health Management Information System, 2011. UNRWA. The Annual Report of the Department of Health 2010. United Nations Relief and Works Agency for Palestine Refugees in the Near East Department of Health (UNRWA): UNRWA, 2011
- World Health Organization. (2003). Oral health promotion: an essential element of a health-promoting school(No. WHO/NMH/NPH/ORH/School/03.3). World Health Organization.
- Abuhaloob, L., & Petersen, P. E. (2018). Oral health status among children and adolescents in governmental and private schools of the Palestinian territories. International Dental Journal, 68(2), 105-112.
- Biscaglia L, di Caccamo P, Terrenato I, Arrica MA, Seita A, Campus G, et al. Oral health status and caries trend among 12-year old Palestine refugee students: results from the UNRWA’s oral health surveys 2011 and 2016. BMC Oral Health 2019; 19(1):157.
- Abuhaloob L, Petersen P. Oral Health Status and Oral Health Behaviour among 5- to 6-year-old Palestinian Schoolchildren – Towards Engagement of Parents and Schoolteachers for Oral Health through Schools. Oral Health Prev Dent 2021; 19(1):673-82.
- Ministry of Health. Health Status in Palestine 2002: Annual Report. Palestine: Ministry of Health-Health Management Information System, 2003
- Abuhaloob, L., & Petersen, P. E. (2023). Health-Promoting Schools Project for Palestine Children's Oral Health. International Dental Journal.
- Petersen PE, Hunsrisakhun J, Thearmontree A, Pithpornchaiyakul S, Hintao J, Jürgensen N, et al. School-based intervention for improving the oral health of children in southern Thailand. Community Dent Health 2015; 32(1):44-50.
- Petersen, P. E., Peng, B., Tai, B., Bian, Z., & Fan, M. (2004). Effect of a school-based oral health education programme in Wuhan City, Peoples Republic of China. International dental journal, 54(1), 33-41.
